Poverty and health are intertwined in the United States. [1] As of 2019, 10.5% of Americans were considered in poverty, according to the U.S. Government's official poverty measure. People who are beneath and at the poverty line have different health risks than citizens above it, as well as different health outcomes. The impoverished population grapples with a plethora of challenges in physical health, mental health, and access to healthcare. These challenges are often due to the population's geographic location and negative environmental effects. Examining the divergences in health between the impoverished and their non-impoverished counterparts provides insight into the living conditions of those who live in poverty.
A 2023 study published in The Journal of the American Medical Association found that cumulative poverty of 10+ years is the fourth leading risk factor for mortality in the United States, associated with almost 300,000 deaths per year. A single year of poverty was associated with 183,000 deaths in 2019, making it the seventh leading risk factor for mortality that year. [2] [3] [4] [5] [6]
Environmental Health Impacts
The environment of people in poverty impacts their health in many aspects. [7] High poverty areas experience problems associated with poor air quality, water pollution, hazardous and toxic waste, and noise pollution. [7] [8] According to Unhealthy Cities: Poverty, Race, and Place in America, poor air quality results in higher rates of children with asthma living in these areas, and nearly 2 million children with asthma live in areas that do not meet national ozone standards. [8] These children are also exposed to greater amounts of allergens that trigger their asthma. [7] Water pollution is also present impoverished cities due which results in unsanitary practices due to poor water supply and sanitation. [9] Impoverished communities are prone to be in proximity to hazardous waste facilities which result in toxic waste dumping, chemical runoff, and water pollution within the area. [8] Because many residents of low-income areas are desperate, they tend to not protest against incoming hazardous facilities. [8] Therefore, these facilities tend to seek out these communities to build in, and this results in more health costs for those in the area. [8] Low-income populations are also more exposed to pesticides, and a significantly higher amount of lead was found in African-American children living in inner-city areas. [7] Neglected Tropical Diseases (NTDs) are also more prevalent in areas of high poverty such as the South and inner-city areas though they often get overlooked by physicians for other diseases. [10]
Climate change also affects the health of those living in low-income communities. Climate change can result in a greater frequency of bad allergy days which results in weakened immune systems and increase asthma cases within the community. [11] From air pollution, respiratory and cardiovascular diseases can worsen due to the greater amounts of chemicals in the atmosphere and hotter temperatures. [11] The warmer temperatures also result in warmer surface water bodies which are better environments for tropical diseases to take root and spread. [11] Climate change also results in a higher frequency of storms, hurricanes, and floods which can result in greater damage to infrastructure resulting in more financial stress for people in low-income communities. [11]
Spatial
Health outcomes of those in poverty can also be determined by spatial, or geographic, location which is another aspect of the environment. Opportunities for healthcare, goods and services like food, and community are all based on geography. [12] Childhood/early adulthood settings highly influence behavior, education, and careers. [12] Those who are financially unstable can usually only find homes that are lower-priced in neighborhoods that are not invested in and are not managed well. [7] These homes are often lower quality, and the costs are higher than what can be managed. [7] According to The Link between Neighborhood Poverty and Wealth: Context or Composition?, Residents in a high-poverty neighborhood reports poor health 1.63 times more than a person in a low-poverty neighborhood, even when controlling for factors like education, marital status, and labor force status. [12] For those living in rural areas, health services are not as accessible, and impoverished people go to doctors fewer times than their counterparts. [1] The effect of spatial location is seen in both physical and mental health.
Poverty and physical health
Poverty can affect health outcomes throughout a person's entire life. The affect may not always be expressed while an individual is impoverished. Mothers who are in poverty during their pregnancies may experience more health risks during their delivery, and their newborn may experience more health risks and markedly more behavioral problems during their development. [13] Furthermore, children in poverty have worse health outcomes during adulthood. This effect is especially pronounced for specific ailments, such as heart disease and diabetes. The impact persists even if a youth escapes poverty by adulthood, suggesting that the stress of poverty encountered during childhood or adolescence has a lasting effect. [14] Previous research has identified the labor environments of the impoverished as more likely to contain risk factors for illness and disability relative to their non-impoverished counterparts. [15] The implication is that the unique stresses of life within an impoverished community contribute to poorer health outcomes, even if the resident does not engage in any specific behavior detrimental to their health. [16] Early into the COVID-19 pandemic in North America, being impoverished was associated with an increased likelihood of contracting COVID-19, as well as dying from it. [17]
Poor housing results in many health problems. Accidents, respiratory disease, and lead poisoning can be caused by poorly built housing. [7] There can also be a lack of safe drinking water, pests, and dampness in the house, and gonorrhea is associated with deteriorating houses. [7] Mothers who live in poverty areas have lower rates of prenatal care and higher rates of infant mortality and low birth weight. [18] Tuberculosis rates are also higher in high-poverty areas. [18] Obesity is associated with poverty due to lack of infrastructure that supports a healthy lifestyle. [19] Often, poverty-areas do not have places to walk or get healthy food nearby, and they are bombarded with unhealthy promotions like cigarettes, alcohol, and fast food. [19] High-poverty areas also had higher death rates than low-poverty areas. [18] [20]
Cost of housing is a huge detriment to physical health. Housing is what the poor pay the most for on a regular basis, and this results in lack of funds for other basic needs like food and health. [7] [19] [21] In a National Health Interview Survey, it was found that around 10% of American families did not receive needed medical care because of cost. [22] Food insecurity also increases due to being unable to buy food due to cost. [23]
According to a 2023 study published in JAMA, cumulative poverty of a decade or more is the fourth leading risk factor for death in the United States annually, being associated with 295,000 deaths. A single year of poverty was associated with 183,000 deaths in 2019, making it the seventh leading risk factor. [4] Up until the age of 40, poor people's survival rates were essentially comparable to those of more affluent people, according to UCR researchers, but after that point, they died at a rate that was noticeably higher. [5] [6]
Poverty and mental health
Poverty also has a complex relationship with mental health. Being in poverty may itself provoke a condition of elevated emotional stress, known as "poverty distress". [24] Poverty is also a precursor or risk factor for mental illness, particularly mood disorders, such as depression and anxiety. Schizophrenia is also strongly associated with poverty, occurring most frequently in the poorest classes of people all over the world, especially in more unequal countries. [25] In a sort of reciprocating relationship, having a mental illness is a major risk factor for being in poverty. Having a mental illness may inhibit a person's ability to work or deter employees from hiring them.
A hypothesis known as " drift hypothesis", posits that for people with psychiatric disorders (primarily schizophrenia), they tend to fall further down the socioeconomic ladder as their condition reduces their functionality. This hypothesis is an effort to establish that people with profoundly limiting psychiatric symptoms are more likely to descend economically, not that the financially challenged are more likely to present severe psychiatric disorders. People experiencing less severe symptoms are less likely to be affected by "drift". [24]

With those in poverty having greater likelihood of suffering from mental illness, the benefit of access to clinical psychotherapy treatments has been explored. Despite numerous barriers for access to care for low-income individuals, there is evidence that those who do receive care respond with significant improvements. This research supports policy measures for improved outreach and access-to-care measures designed to benefit those with low-incomes and mental health disorders. [26]
Mental health is affected by location as well. Noisy housing impacts reading in children and promotes psychological stress. [7] Many poor families move more often and are residentially instable. This results in children experiencing instability with relationships with peers. [7] They also experience more stressful life events which places strain on their mental state as the events cumulate. [7] [11] As both parents and children try to cope, they may cut themselves off from social interactions and healthy development. [7]
Race and health
Poverty and race both impact the health outcome of a person. [18] Of the residents in poverty-areas, well over half are people of color. [18] When compared to White Americans, all other races have lower outcomes of infant mortality, low birth weight, prenatal care, and deaths in cities. [18] People of Color have an 80% higher mortality rate than White people, and this includes deaths from cancer, accidents/ homicides, and disease. [1] Those in severe poverty are more likely to be Black Americans and Latinx. [19] More than one-fourth of the Native American and Alaska Native population lives in poverty. [27] When adjusted for age, the death rate of Native Americans and Alaska Natives is 40% higher than the general population, and 39% of the children are obese or overweight. [27] Mental health is the number one problem in the Native American and Alaska Native population. [27] For Black Americans, racial segregation in neighborhoods are barriers for equitable health opportunities. [7] Most current neighborhoods that are predominantly Black have been institutionally disinvested and have fewer public services and more housing insecurity. [7] With these barriers, many Black Americans do not have the wealth of a family home passed down through generations. [7] Latinx and Asians may also have trouble with home ownership due to cultural and linguistic isolation. [7]
Homelessness and health
Homelessness is a public welfare and health epidemic within the United States. Any period of homelessness is associated with adverse health consequences. [28] These adverse health consequences are associated with poor living conditions and a lack of access to treatment facilities. Due to living in extreme poverty it is unlikely for an individual or a family to have a healthcare plan. These healthcare plans are important in obtaining treatment for illnesses or injury from treatment facilities. Without it, individuals and families are left to deal with their ailments themselves or endure further financial burden by receiving treatments without a health insurance plan. Respiratory infections and outbreaks of tuberculosis and other aerosol transmitted infections have been reported. Homeless intravenous drug users are at an increased risk of contracting HIV, and hepatitis B and C infections.
[29] The close living spaces of areas such as Skid Row in California provide an environment in which infectious diseases can spread easily. These areas with a high concentration of homeless individuals are dirty environments with little resources for personal hygiene. It was estimated in a report to congress that 35% of homeless were in unsheltered locations not suitable for human habitation. [30]
There is a bidirectional relationship between homelessness and poor health. [31] Homelessness exacts a heavy toll on individuals and the longer individuals experience homelessness, the more likely they are to experience poor health and be at higher risk for premature death. [32] Health conditions, such as substance use and mental illness, can increase people's susceptibility to homelessness. Conversely, homelessness can further cause health issues as they come with constant exposure to environmental threat such as hazards of violence and communicable diseases. Homeless people have disproportionately high rates of poly substance use, mental illness, physical health problems and legal issues/barriers in attaining employment. [33]
Large number of homeless people work but few homeless people are able to generate significant earnings from employment alone. [34] Physical health problems also limit work or daily activities which are barriers to employment. Substance use is positively associated with lower work level but is negatively related to higher work level. [35] Those with physical health problems are substantially more likely than those with mental health problems to be in the more generous disability programs. Substance use disorders are also a barrier to participation in disability programs. Rates of participation in government programs are low, and people with major mental disorders have low participation rate in disability programs. [36]
Around the United States, homeless deaths surged 77% from 2016 to 2020. An analysis from The Guardian in February 2022 found that some 18,000 homeless people died on the streets and in encampments and shelters over a five year period, with 5,000 of these deaths occurring in 2020. The non-profit National Health Care for the Homeless Council places homeless deaths at between 17,000 and 40,000 annually, as many are never counted given the federal government does not track homeless deaths nationally. The top direct causes of death among the homeless population include "drug overdoses, violence, traffic deaths and premature lethality of treatable conditions like heart disease." Regarding drug deaths, methamphetamine is a significant killer, as people who are homeless use the stimulant drug to stay awake and alert in order to protect themselves from violence. The report also notes that, outside of direct medical causes of death, a major factor contributing to both the epidemic of homelessness and surge in deaths among the homeless population is the lack of affordable housing throughout much of the country. [37]
Homelessness among the elderly has been increasing. [38] The Los Angeles County Department of Public Health found that homeless persons die at greater rates than the general public from specific causes. [39] They are more likely to die by: 35 times from alcohol or drug overdoses, 16 times from auto accidents, 14 times from murder, 8 times from suicide, and 4 times from heart disease. [39] According to data from HUD in September 2023, the elderly are now the fastest growing demographic of the homeless population. [40]
Judge Milan Smith Jr., an American jurist claimed that homelessness is "presently the defining public health and safety crisis in the western United States." [41] According to the Lahsa data, on average six unhoused people are dying each day. the causes reported of death are Overdoses, heart disease, traffic accidents, homicides, hypothermia, and heat exhaustion.Va Lecia Adams Kellum, Lahsa's CEO, believes "The primary causes of homelessness are economic." [42]Health care policy
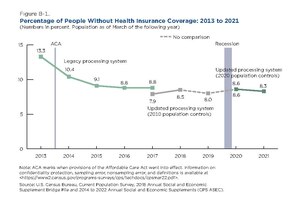
Between 1987 and 2005, the number of people without health insurance in the United States rose from just over 30 million, to 46.6 million. [43] Insurance tends to increase the price of services, [9] and at that time, 8.5% of people belonging to households that made over $75,000 annually were uninsured. For families earning $25,000 or less, that percentage rose to 24.4% uninsured. [43] This figure exhibits how lack of access to care via health insurance disproportionately affects those in poverty.
Despite the cost of healthcare being an obstacle for those with relatively low incomes, research suggests that insurance coverage will not dramatically change outcomes related to physical health. Access to Medicaid for low-income adults aided in the diagnosis of metabolic disease, saw a reduction in diagnosis of mental health disorders, and reduced incurrence of "catastrophic medical costs" by patients dramatically. While these positive effects were observed, outcomes for heart disease, diabetes, and other physical health characteristics were not meaningfully improved. It has been posited that one year, the duration of the study, is an insufficient length to fully observe the divergent health outcomes that would be characteristic of an experiment with a lengthier time-table. [44] Also, minorities have an excess amount of deaths due to diseases like cancer and cardiovascular disease compared to whites. [1]
The medical-industrial complex also contributes to the difficulties of patients paying for medications and healthcare costs. [45]
Actions taken by the government
The United States government has passed acts to make healthcare more accessible. [46] Though it does not have universal health coverage, the country has two forms of public insurance, Medicare and Medicaid. Medicare is insurance for those who are over 65 or have long-term disabilities or end-stage renal disease. [46] Medicaid allows for federal funding to match health care services and allow low-income families, low-income pregnant women, low-income children up to 18 years old, the blind, and those with disabilities to have these services. [46] Medicaid is administered by states, so states have the right to set the criteria for eligibility. According to The Commonwealth Fund website, Medicaid now covers 17.9% of Americans. The Children's Health Insurance Program (CHIP) provides insurance to children in low-income families and covers 9.6 million children, according to The Commonwealth Fund. [46] The Affordable Care Act was passed in 2010, and it expanded Medicaid eligibility and provided funding for federally qualified health centers. These centers take patients regardless of ability to pay and provides free vaccines to uninsured and underinsured children. [46] Community mental health services are also funded by the federal government through grants provided to states by the Substance Abuse and Mental Health Services Administration. [46]
Recommendations to further improve healthcare access
One recommendation to address the inequity of healthcare for the poor is to take community-based action. [1] [47] One example of this is county health councils in Tennessee. These are volunteer groups from the community who assess health inequities within their county and decide what policies to implement. [47] Another idea is to implement community-oriented primary care where physicians consider the environment and culture of the patient to further their health. [1] To improve housing, weatherization programs are recommended to refurbish poor housing to be more health friendly. [21]
Policy wise, it is recommended to continue investing in the health of the poor by creating an amendment or law and increasing affordable housing. [11] [48] The amendment would ensure that adequate housing is a right to be enjoyed by everyone, and if that could not happen, then a law could be passed for a better housing policy. [11] Affordable housing can be increased by increasing subsidies through housing vouchers for households or reduced interest loans for developers.
References
- ^ a b c d e f Patrick, Donald L.; Stein, Jane; Porta, Miquel; Porter, Carol Q.; Ricketts, Thomas C. (1988). "Poverty, Health Services, and Health Status in Rural America". The Milbank Quarterly. 66 (1): 105–136. doi: 10.2307/3349987. JSTOR 3349987. PMID 3262817.
- ^ Brady, David; Kohler, Ulrich; Zheng, Hui (2023). "Novel Estimates of Mortality Associated With Poverty in the US". The Journal of the American Medical Association. 183 (6): 504–628. doi: 10.1001/jamainternmed.2023.0276. PMC 10111231. PMID 37067817.
- ^ Danelski, David (April 17, 2023). "Poverty is the 4th greatest cause of U.S. deaths". UC Riverside News. Retrieved June 23, 2023.
- ^ a b Barber, William; Gonsalves, Gregg (June 22, 2023). "The fourth leading cause of death in the US? Cumulative poverty". The Guardian. Retrieved June 27, 2023.
- ^ a b Hughes, Clyde (April 17, 2023). "Poverty is fourth-largest cause of U.S. deaths, researchers say". United Press International. Retrieved July 2, 2023.
- ^
a
b Jarow, Oshan (July 14, 2023).
"Poverty is a major public health crisis. Let's treat it like one". Vox. Retrieved August 24, 2023.
A single year of poverty, defined relatively in the study as having less than 50 percent of the US median household income, is associated with 183,000 American deaths per year. Being in 'cumulative poverty,' or 10 years or more of uninterrupted poverty, is associated with 295,000 annual deaths.
- ^ a b c d e f g h i j k l m n o p q Saegert, Susan; Evans, Gary W. (July 2003). "Poverty, Housing Niches, and Health in the United States: Poverty, Housing Niches, and Health". Journal of Social Issues. 59 (3): 569–589. doi: 10.1111/1540-4560.00078.
- ^ a b c d e Fitzpatrick, Kevin; Lagory, Mark (2013). Unhealthy Cities. doi: 10.4324/9780203843765. ISBN 978-1-136-91529-1.[ page needed]
- ^ a b Wagstaff, Adam (2022-09-01). "Poverty and Health Sector Inequalities". Bulletin of the World Health Organization. 100 (9). doi: 10.2471/blt.00.000922.
- ^ Hotez, Peter J. (2020). "The United States of America". Poverty and the Impact of COVID-19: The Blue-Marble Health Approach. Johns Hopkins University Press. pp. 12–39. ISBN 978-1-4214-4050-7. Project MUSE chapter 2625177.
- ^ a b c d e f g Tonn, Bruce; Hawkins, Beth; Rose, Erin; Marincic, Michaela (August 2021). "A futures perspective of health, climate change and poverty in the United States". Futures. 131: 102759. doi: 10.1016/j.futures.2021.102759. S2CID 236380875.
- ^ a b c Do, D. P.; Finch, B. K. (2008-07-15). "The Link between Neighborhood Poverty and Health: Context or Composition?". American Journal of Epidemiology. 168 (6): 611–619. doi: 10.1093/aje/kwn182. PMC 2584357. PMID 18687664.
- ^ Larson, Charles P (October 2007). "Poverty during pregnancy: Its effects on child health outcomes". Paediatrics & Child Health. 12 (8): 673–677. doi: 10.1093/pch/12.8.673. PMC 2528810. PMID 19030445.
- ^ Raphael, Dennis (May 2011). "Poverty in childhood and adverse health outcomes in adulthood". Maturitas. 69 (1): 22–26. doi: 10.1016/j.maturitas.2011.02.011. PMID 21398059.
- ^ Murray, S. (28 March 2006). "Poverty and health". Canadian Medical Association Journal. 174 (7): 923. doi: 10.1503/cmaj.060235. PMC 1405857. PMID 16567753.
- ^ Haan, Mary; Kaplan, George A.; Camacho, Terry (June 1987). "Poverty and Health Prospective Evidence from the Alameda County Study". American Journal of Epidemiology. 125 (6): 989–998. doi: 10.1093/oxfordjournals.aje.a114637. hdl: 2027.42/51456. PMID 3578257.
- ^ Finch, W. Holmes; Hernández Finch, Maria E. (2020). "Poverty and Covid-19: Rates of Incidence and Deaths in the United States During the First 10 Weeks of the Pandemic". Frontiers in Sociology. 5: 47. doi: 10.3389/fsoc.2020.00047. PMC 8022686. PMID 33869454.
- ^ a b c d e f Ventura, Stephanie J. (1975). Selected Vital and Health Statistics in Poverty and Nonpoverty Areas in 19 Large Cities, United States, 1969-71 (PDF). U.S. Government Printing Office. ISBN 978-0-8406-0049-3. OCLC 1015648361.[ page needed]
- ^ a b c d Woolf, S; Johnson, R; Geiger, H (October 2006). "The Rising Prevalence of Severe Poverty in AmericaA Growing Threat to Public Health". American Journal of Preventive Medicine. 31 (4): 332–341.e2. doi: 10.1016/j.amepre.2006.06.022. PMID 16979459.
- ^ Ram, Rati (December 2005). "Income inequality, poverty, and population health: Evidence from recent data for the United States". Social Science & Medicine. 61 (12): 2568–2576. doi: 10.1016/j.socscimed.2005.04.038. PMID 15963618.
- ^ a b Tonn, Bruce; Hawkins, Beth; Rose, Erin; Marincic, Michaela (March 2021). "Income, housing and health: Poverty in the United States through the prism of residential energy efficiency programs". Energy Research & Social Science. 73: 101945. Bibcode: 2021ERSS...7301945T. doi: 10.1016/j.erss.2021.101945. S2CID 233846605.
- ^ Martinez, Michael E.; Clarke, Tainya C. (2020). "Percentage of Families That Did Not Get Needed Medical Care Because of Cost, by Poverty Status--National Health Interview Survey, United States, 2013 and 2018". Morbidity and Mortality Weekly Report. 69 (23): 727. doi: 10.15585/mmwr.mm6923a4. PMC 7315793. PMID 32525851.
- ^ Gundersen, Craig; Hake, Monica; Dewey, Adam; Engelhard, Emily (2021). "Food Insecurity during COVID-19". Applied Economic Perspectives and Policy. 43 (1): 153–161. doi: 10.1002/aepp.13100. PMC 7537061. PMID 33042509.
- ^ a b Kuruvilla, A.; Jacob, K. S. (October 2007). "Poverty, social stress & mental health". Indian Journal of Medical Research. 126 (4): 273–279. PMID 18032802. Gale A173276699 ProQuest 195977890.
- ^ Read, John (July 2010). "Can poverty drive you mad? 'schizophrenia', socio-economic status and the case for primary prevention". New Zealand Journal of Psychology. 39 (2): 7–20. Gale A243877211 ProQuest 872020933.
- ^ Santiago, Catherine DeCarlo; Kaltman, Stacey; Miranda, Jeanne (February 2013). "Poverty and Mental Health: How Do Low-Income Adults and Children Fare in Psychotherapy?: Poverty and Mental Health". Journal of Clinical Psychology. 69 (2): 115–126. doi: 10.1002/jclp.21951. PMID 23280880.
- ^ a b c Sarche, Michelle; Spicer, Paul (June 2008). "Poverty and Health Disparities for American Indian and Alaska Native Children: Current Knowledge and Future Prospects". Annals of the New York Academy of Sciences. 1136 (1): 126–136. Bibcode: 2008NYASA1136..126S. doi: 10.1196/annals.1425.017. PMC 2567901. PMID 18579879.
- ^ Fusaro, Levy (2018). "Racial and Ethnic Disparities". Demography. 55 (6): 2119–2128. doi: 10.1007/s13524-018-0717-0. PMC 7665902. PMID 30242661. S2CID 52315072.
- ^ Roy, L.; Crocker, A. G.; Nicholls, T. L (2014). "Criminal Behavior and Victimization Among Homeless". Psychiatr Serv. 65 (6): 739–50. doi: 10.1176/appi.ps.201200515. PMID 24535245. S2CID 26616742.
- ^ Henry, M.; Morrill, T. "The 2018 Annual Homeless Assessment Report (AHAR) to Congress" (PDF). HUD Exchange. Archived (PDF) from the original on March 30, 2020. Retrieved May 30, 2019.
- ^ Lippert, Adam M.; Lee, Barrett A. (2015). "Stress, Coping, and Mental Health Differences among Homeless People". Sociological Inquiry. 85 (3): 343–374. doi: 10.1111/soin.12080.
- ^ Quigley JM, et al. (2001). Homelessness in California. Public Policy Institute of California (Report). S2CID 153541613.
- ^ Fitzpatrick, Kevin Michael (2013). Poverty and Health: A Crisis Among America's Most Vulnerable [2 volumes]: A Crisis among America's Most Vulnerable. ABC-CLIO. p. 165. ISBN 978-1-4408-0264-5. Archived from the original on February 22, 2023. Retrieved February 8, 2019.
- ^ Zuvekas, Samuel H.; Hill, Steven C. (2000). "Income and employment among homeless people: the role of mental health, health and substance abuse". The Journal of Mental Health Policy and Economics. 3 (3): 153–163. CiteSeerX 10.1.1.490.6983. doi: 10.1002/mhp.94. PMID 11967451.
- ^ "Baggett, Travis P, and Darlene M Jenkins. "Chapter 6." Poverty and Health: A Crisis among America's Most Vulnerable, vol. 1, ABC-CLIO, LLC" (PDF). Archived (PDF) from the original on October 6, 2017. Retrieved October 5, 2017.
- ^ "Affordable housing, homelessness, and mental health: What health care policy needs to address. - Free Online Library". thefreelibrary.com. Archived from the original on September 7, 2018. Retrieved September 6, 2018.
- ^ McCormick, Erin (7 February 2022). "'Homelessness is lethal': US deaths among those without housing are surging". the Guardian. Retrieved 24 May 2023.
-
^ Grabenstein, Hannah (March 3, 2023).
"More seniors are becoming homeless, and experts say the trend is likely to worsen". PBS. Retrieved June 16, 2023.
There's no single reason for the rise in the older homeless population. Weak social safety nets, mass incarceration policies and an insufficient supply of affordable housing are among the many factors
- ^
a
b Fuller, Thomas (April 18, 2022).
"A Rising Tally of Lonely Deaths on the Streets".
The New York Times.
A study by the Los Angeles County Department of Public Health found that homeless people are 35 times as likely as the general population to die of a drug or alcohol overdose. They are also four times as likely to die of heart disease, 16 times as likely to die in a car crash, 14 times as likely to be murdered and eight times as likely to die of suicide.
-
^ Louis, Serah (September 23, 2023).
"'Unconscionable': Baby boomers are becoming homeless at a rate 'not seen since the Great Depression' — here's what's driving this terrible trend".
Yahoo! Finance. Retrieved September 23, 2023.
Thanks in part to a series of recessions, high housing costs and a shortage of affordable housing, older adults are now the fastest-growing segment of America's homeless population, according to a report in the Wall Street Journal, based on data from the Department of Housing and Urban Development.
- ^ Rector, Kevin (July 6, 2023). "9th Circuit conservatives blast homelessness ruling, say issue is 'paralyzing' U.S. West". The Los Angeles Times. Retrieved 9 July 2023.
- ^ Levin, Sam (June 29, 2023). "Los Angeles unhoused population reaches 75,000 amid humanitarian crisis". The Guardian. Retrieved 9 July 2023.
- ^ a b DeNavas-Walt, Carmen; Proctor, Bernadette D.; Lee, Cheryl Hill (August 2006). Income, Poverty, and Health Insurance Coverage in the United States: 2005. US Census Bureau.[ page needed]
- ^ Baicker, Katherine; Taubman, Sarah L.; Allen, Heidi L.; Bernstein, Mira; Gruber, Jonathan H.; Newhouse, Joseph P.; Schneider, Eric C.; Wright, Bill J.; Zaslavsky, Alan M.; Finkelstein, Amy N. (2 May 2013). "The Oregon Experiment — Effects of Medicaid on Clinical Outcomes". New England Journal of Medicine. 368 (18): 1713–1722. doi: 10.1056/NEJMsa1212321. PMC 3701298. PMID 23635051.
- ^ Wohl, Stanley. The Medical Industrial Complex / Stanley Wohl. First edition. New York: Harmony Book, 1984: 100-234
- ^ a b c d e f "United States". www.commonwealthfund.org. 2020-06-05. Retrieved 2023-04-05.
- ^ a b Erwin, Paul Campbell (September 2008). "Poverty in America: How Public Health Practice Can Make a Difference". American Journal of Public Health. 98 (9): 1570–2. doi: 10.2105/AJPH.2007.127787. PMC 2509587. PMID 18633082.
- ^ Bor, Jacob; Cohen, Gregory H; Galea, Sandro (April 2017). "Population health in an era of rising income inequality: USA, 1980–2015". The Lancet. 389 (10077): 1475–1490. doi: 10.1016/S0140-6736(17)30571-8. PMID 28402829. S2CID 13760884.